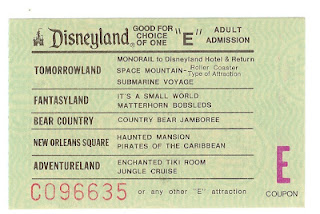
Disneyland's coveted "E" ticket -
Have you ever had something that you really, really looked forward to doing?
I’m not talking about going on the same vacation that you have done several times. I’m talking about something that you believe will change your life in a good way. I had one of those when I was about 10 years old. I was going to go to my first amusement park, Coney Island in Cincinnati. If you are from the area, you are likely familiar with Kings Island, which was created to take the place of Coney Island. I believed that this would be the greatest thing that would ever happen to me.
We were not a family with a lot of money. I never wanted for much, but this was going to be a real splurge. So, we make the hour drive to Cincinnati and find out that you had to buy a book of coupons to ride certain classes of rides, similar to what Disney did with the "E" ticket for their premiere rides in the '70s. The only problem was that you were limited on tickets for the best rides and had to ride the little kiddie rides to use up the lesser coupons. In the end, it was OK but certainly not the adventure that I had convinced myself it would be. My life had not changed.
When we last spoke, I was a couple weeks post-kidney transplant and I was escorting my dialysis machine out the door. I was feeling great and life was good. However, later that week, I had to get the stent removed that had been placed in my ureter between the kidney and bladder to heal the transplant connection. The young doctor seemingly hadn’t done many of these and struggled getting it out. I will spare you the details but within a week I had a UTI and it was just the beginning of my complications.
Over the next few months, I contracted a number of infections and had two short stays in the hospital. Four months in, the transplant committee decided that I needed to have a nephrostomy. For those of you that are lucky enough to never have one of these, a nephrostomy is a procedure where they place a tube directly into the kidney, run it through your side into a bag. I have a discreet bag that is hidden under my pants so I can get out in public. I have a large bag that can hold up to 2 liters of urine to get through the night.
So, for the last three months, Julia and I have a routine that every morning she takes the large bag off and attaches the small bag. She has to tape me up with gauze because the hole in my side never really heals and has some seepage every day. Then at night, we move from the small bag to the larger bag. Because I have to drink at least three liters of water each day, I am constantly emptying the small bag.
It was determined after a myriad of tests that the connection of the ureter to my bladder had a problem. It seems that a small section of the ureter had pretty much shriveled up and nearly died. There was an issue with scar tissue at the juncture. As a result, urine has backing up into my kidney and potentially damaging it. This was the culprit of my infections. The nephrostomy gave me a short-term fix for that problem.
Needless to say, my kidney transplant has turned into my trip to Coney Island. In some ways, the transplant has been good but in other ways it has been disappointing. Don’t get me wrong, I am glad we did it as it has given me back 20+ hours every week that I don’t have to spend attached to a dialysis machine. I have much more freedom in my diet and fluid consumption. We were even able to have a little vacation escape to Northern Arizona free of treatments and medical procedures, which is something we hadn’t done in almost 6 years. Other than the week “up North,” my weekly tests, labs and appointments have had to continue which we didn’t expect.
Wednesday will be a big day for me with another major surgery to fix the ureter. They will go in, detach the ureter from the bladder, clip off the damaged section and then reattach it in a different spot. If all goes well, the nephrostomy tube can be removed, the healing with resume and in two months I’m at 100%. This will be like walking into Coney Island and having someone hand me free tickets to ride the roller coaster.









.jpg)